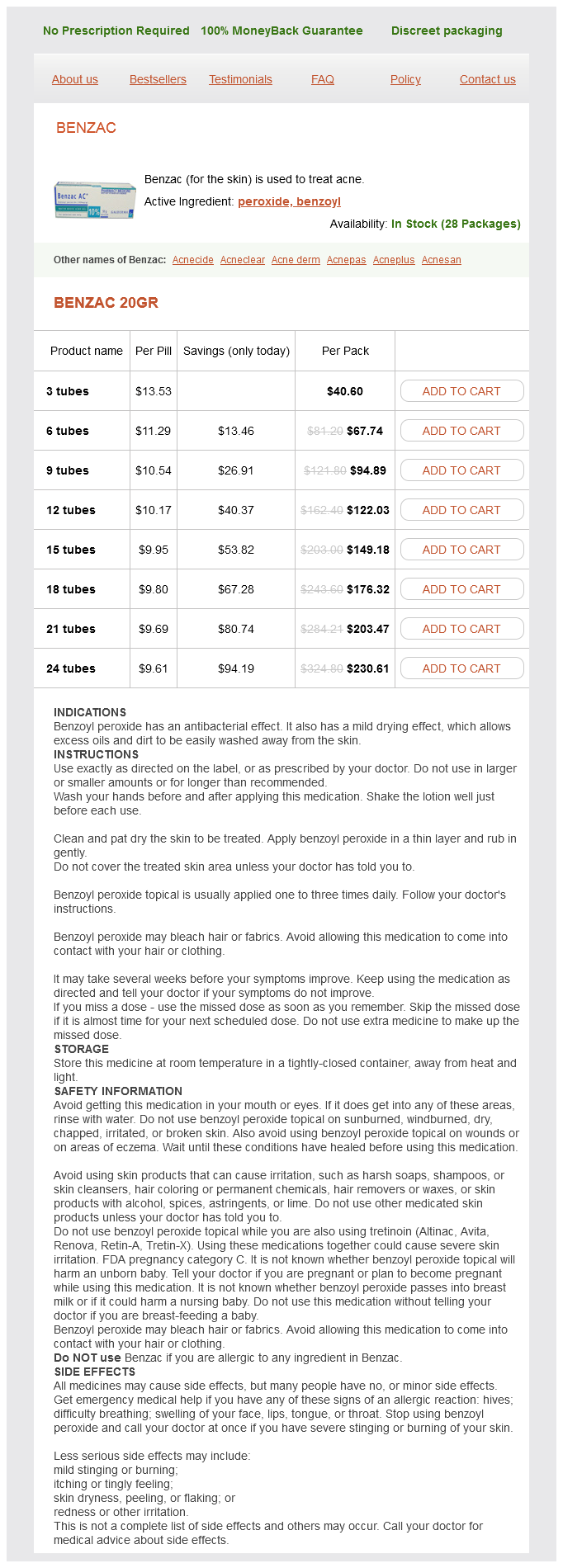
Benzac
Benzac 20gr
- 3 tubes - $40.60
- 6 tubes - $67.74
- 9 tubes - $94.89
- 12 tubes - $122.03
- 15 tubes - $149.18
- 18 tubes - $176.32
- 21 tubes - $203.47
- 24 tubes - $230.61
Likewise skin care steps buy benzac 20 gr without prescription, stating "I am going to touch you now" is helpful in alleviating surprises. Using these statements demonstrates that the examination is a cooperative effort, further empowering the patient in facilitating care. Positioning the patient for examination begins with the elevation of the head of the examining table to approximately 30° from horizontal. This 39 serves three purposes: 1) it allows eye contact between the patient and physician and facilitates communication between the patient and physician during the entire examination; 2) it relaxes the abdominal wall muscle groups, making abdominal and pelvic examinations easier; and 3) it allows the physician to observe the patient for responses to the examination, which may provide valuable information. The physician should sit at the foot of the examining table, with the examination lamp adjusted to shine on the perineum. After contact with the patient, there should be minimal contact with equipment such as the lamp. Inspection and Examination of the External Genitalia 40 the pelvic examination begins with the inspection and examination of the external genitalia. Inspection should include the mons pubis, labia majora, labia minora, perineum, and perianal area. Inspection continues as palpation is performed in an orderly sequence, starting with the clitoral hood, which may be pulled back to inspect the glans proper. The labia are spread laterally to allow inspection of the introitus and outer vagina. The urethral meatus and the areas of the urethra and Skene glands should be inspected. The sequence of inspection and then palpation should be included in the thorough examination of the external genitalia. The forefinger is placed an inch or so into the vagina to gently milk the urethra. The forefinger is then rotated posteriorly to palpate the area of the Bartholin glands between that finger and the thumb. The Pederson speculum works well for most nulliparous women and for postmenopausal women with atrophic, narrowed vaginas. The Graves speculum has blades that are wider, higher, and curved on the sides; it is more appropriate for most parous women. Its wider, curved blades keep the looser vaginal walls of multiparous women separated for visualization. A Pederson speculum with extra narrow blades may be used for visualizing the cervix in pubertal girls. Selection of the correct type of speculum is a key aspect of the comfortable and complete speculum examination. Warming the speculum is done for the comfort of the patient and to aid with insertion. Until recently, the use of lubricants was avoided because of interference with cytologic interpretation, although this is less of a concern with liquidbased Pap test techniques. Situations that may require lubricant use are encountered infrequently and include examination of some prepubertal girls, some postmenopausal women, and patients with irritation or lesions of the vagina.
A: this low-magnification view demonstrates markedly thickened and inflamed peritoneal tissue top half) that is densely adherent to the appendix bottom half) skin carecom cheap 20 gr benzac with visa. Islands of keratin flakes with associated inflammation are located near the peritoneal surface at the top of the image. B: At high magnification, loosely aggregated keratin flakes asterisk are seen in association with a mixed inflammatory infiltrate that includes multinucleated giant cells a~Tmlf1. In these three cross sections of a fallopian tube from a postpartum tubal ligation. Endosalpin· giotic glands are also referred to as benign mullerian glandu· lar inclusions or mullerian inclusion cysts. Endosalpingiosis is most common in the reproductive age group, occurs almost exclusively in women, and is found in about 10% to 15% of pelvic lymph node dissections and surgically removed omenta. It is often found in association with inflammatory tubal disease and epithelial ovarian tumors, most notably serous bordedine tumors. Endosalpingiosis may be derived from dislodged cells originating from the 6mbria of the f. The tubal-type glands of endosalpingiosis are of variable size and shape, may be dilated. A small nodule of decidual ized cells is present within submesothelial omental tissue. Although most investigators interpret the frequent associ· ation of endosalpingiosis and serous borderline tumor within a lymph node as evidence that the former may serve as an intranodal precursor of the latter,31 one group has speculated that the endosalpingiotic glandular inclusions may represent morphologically uninformative metastases of serous border· line turnor. The glands of endosalpingiosis tend to be architecturally simple, although minor papillary infoldings may be pn:sent. When psammoma bodies arc found intermingled with subserosal6brous tissue in the absence ofassociated epithelial elements, "burned-out" endosalpingiosis is the presumptive diagnosis. Endosalpingiosis is usually an incidental microscopic finding or visible as millimeter-sized cystic bumps on serosal surfaces, but can create a tumor-like mass when florid and cystic. Differential Diagnosis In contrast to endometriosis, the glands of endosalpingiosis arc not associated with endometrial·type stroma or evidence of prior hemorrhage. The mesonephric tubules of mesonephric remnants, which are typically found in the broad ligament, arc distinguished from endosalpingiosis by their coUarettes of smooth muscle and lack of ciliated cells. A: the benign glands have a simple architecture and are lined by tubal-type epithelium. This "burned-out" focus in the uterine subserosa consists of fibrous tissue and psammoma bodies. Endocervicosis typically occurs in women of reproductive age, may he associated with pelvic pain or site·spccmc symptoms, and may form a visible mass.
Retained placenta acne hoodie 20 gr benzac purchase visa, genital tract trauma, lacerations, and coagulation disorders are other causes. If this finding is confirmed, oxytocin infusion should be increased and either methylergonovine maleate or prostaglandins administered if excessive bleeding continues. Such measures include large-bore intravenous access; rapid crystalloid infusions; type, 321 cross-match, and administration of blood or blood components as needed; periodic assessment of hematocrit and coagulation profile; and monitoring of urinary output. There has been a shift in philosophy regarding transfusion of blood products in the setting of active hemorrhage, with greater willingness to intervene earlier and prevent coagulopathy rather than to delay treatment until coagulopathy is diagnosed. Depending on the clinical scenario, the use of laboratory measurements to guide transfusion of plasma, cryoprecipitate, and platelets may be reasonable. The recent recommendation to avoid transfusion in stable, asymptomatic hospitalized patients with a hemoglobin >7 to 8 mg/dl does not apply in the setting of postpartum hemorrhage. This muscular contraction, rather than coagulation, prevents excessive bleeding from the placental implantation site. The clinical diagnosis of atony is based largely on the tone of the uterine muscle on palpation. Instead of the normally firm, contracted uterine corpus, a softer, more pliable-often called "boggy"-uterus is found. Frequently, the uterus contracts briefly when massaged, only to become relaxed again when the manipulation ceases. Because hemorrhage can occur in the absence of atony, other etiologies must be sought in the presence of a firm fundus. Management of Uterine Atony Management of uterine atony is both preventive and therapeutic. The protocol for management of the third stage includes oxytocin infusion (usually 20 units in 1 L of normal saline infused at 200 to 500 mL/hour) initiated immediately following delivery of the infant or its anterior shoulder, gentle cord traction, and uterine massage. Some physicians do not begin oxytocin infusion until after delivery of the placenta to avoid placental entrapment; however, there is no firm evidence that the rates of entrapment are higher with active management than with other strategies. Immediate breastfeeding may also enhance uterine contractility and, thus, reduce blood loss. Once uterine atony is diagnosed, management can be categorized as medical, manipulative, or surgical. Management must be individualized in cases of severe uterine atony, taking into account the extent of hemorrhage, the overall status of the patient, and her future childbearing desires (see Box 12. Bimanual uterine massage alone is often successful in causing uterine contraction, and this should be done while preparations for other treatments are under way.
Lemon Pectin (Pectin). Benzac.
- How does Pectin work?
- Are there safety concerns?
- What is Pectin?
- What other names is Pectin known by?
- Are there any interactions with medications?
- High cholesterol.
- Dosing considerations for Pectin.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96506
Syndromes
- Knee swelling
- Make sure you have realistic expectations from the surgery.
- The surgeon makes a small (1 to 1-1/2 inch) incision (cut) on your back and moves the back muscles away from the spine. The doctor uses a special microscope to see the problem disk or disks and nerves during surgery.
- Bloody fluid or pus inside the middle ear
- Convulsions
- Oxycodone (Percocet or Oxycontin)
- Milk-colored peritoneal fluid may be a sign of carcinoma, cirrhosis of the liver, lymphoma, tuberculosis, or infection.
- A cough that produces more than a few teaspoons of blood
- The results of tests
Usage: q.i.d.
Additional information: